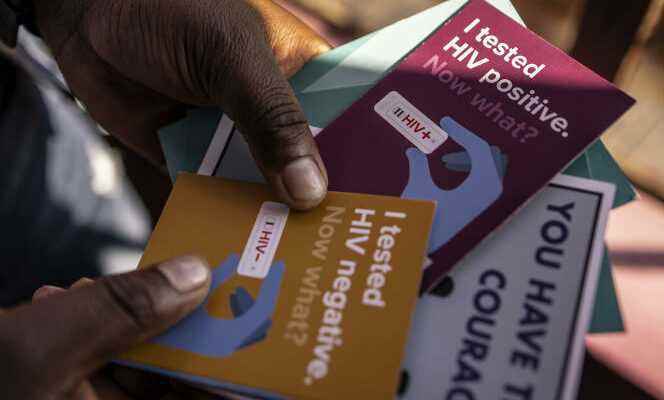
For the African continent, these are hopeful experiences. That of reaching by 2030 the objective set by UNAIDS of the “three 95s”: 95% of people living with HIV knowing their serological status, 95% of infected people on long-term antiretroviral (ARV) treatment and 95 % of people on treatment with an undetectable viral load and therefore not contagious.
In Kenya, for five years, Médecins sans frontières (MSF) carried out the ambitious pNdhiwa project, in the county of Homa Bay (east), with more than 6,000 inhabitants. A study published at the end of 2020 about this experiment confirmed how the mobilization of an entire community, from prevention to screening and support in care, could make it possible to extinguish an outbreak of HIV in one of the areas. the most contaminated in Africa. The three objectives set by UNAIDS have been exceeded.
In Eswatini, the Global Fund to Fight AIDS, Tuberculosis and Malaria conducted a similar program based on needs in the field with the most vulnerable populations: women and adolescent girls. With success: this small southern African country of just over a million inhabitants has achieved the feat of becoming, at the end of 2020, after Switzerland, the second country to reach the “three 95s”.
The “catastrophic repercussions” of SARS-CoV-2
Yet the continent continues to pay the highest price for the pandemic. Since the discovery of the first case in the 1980s, of the 36.3 million deaths reported worldwide, seven out of ten are African. And the SARS-CoV-2 pandemic has not helped matters with its curfews, lockdowns and disruptions in the supply of drugs, condoms and tests, diverting part of the human effort and budget granted for more than thirty years by the States and international solidarity.
A “heavy impact”explain to World Peter Sands, head of the Global Fund, “with catastrophic repercussions”. For the first time, he explains, “in 2020, the main prevention and screening services recorded significant declines”, which must be countered ” urgently ” by an international political and financial upheaval. Without it, 7.7 million people will die in the next ten years from AIDS and opportunistic diseases. The outcome, in early 2023, of the seventh replenishment of the resources of the Global Fund, which provides a quarter of the global funding for control programs, will set the tone. At least 18 billion dollars (more than 17 billion euros) are deemed necessary to help governments “to save 20 million lives and reduce the death rate from HIV alone by 68%”, emphasizes Peter Sands.
In 2021, three quarters of people living with the virus are on ARV treatment, including on the African continent
However, considerable progress has been made in recent decades. It was under the chairmanship of the Ghanaian Kofi Annan, Secretary General of the United Nations from 1997 to 2006, that the Global Fund was created at the African Union summit in Abuja (Nigeria) in 2001. It was to give resources and consistency to the fight against a disease that was decimating the continent as a priority. The scientific community, the NGOs and the militant collectives have weighed with all their weight on the laboratories to bring down the exorbitant cost of triple therapy. It only costs 66 dollars (about 65 euros) per year and per patient today, compared to more than 10,000 dollars when it was developed in 1996.
“For several years, access to antiretrovirals has been very good in Africa, testifies Pierre Mendiharat, deputy director of operations at MSF. Thanks to the financing mechanisms of the Global Fund and the American agency PEPFAR [Plan présidentiel d’urgence d’aide à la lutte contre le sida ], to group purchases, to the arrival of generics, to competition which has promoted transparency. »
Mother-to-child transmission has been stopped
Since the peak reached in 2004, the pandemic has been decreasing. Mortality has halved: in 2020, “only” 680,000 people died of HIV-related causes worldwide, including around 500,000 in Africa. In 2021, three quarters of people living with the virus are on ARV treatment, including on the continent. Mother-to-child transmission has been halted, preventive treatment (PrEP) given to high-risk populations, such as sex workers, injecting drug users and people in same-sex relationships, has expanded. “The continent’s healthcare systems, despite their fragility, have adapted, explains Pierre Mendiharat again. We manage to reach tens of thousands of patients. And the tipping point towards a possible way out of the crisis was, in July 2011, the scientific demonstration of the undetectable viral load. However, we need to find a new impetus. »
Indeed, women and adolescent girls – the first victims of sexual violence and therefore the most contaminated –, as well as all people discriminated against for their sexual choices or identity, remain very vulnerable. And the fear of AIDS continues to kill, especially in African countries that criminalize homosexuality or transidentity. Resistance to screening and acceptance of the disease keeps HIV-positive people away from care and masks part of the scourge. It is estimated that approximately 30% of patients Africans do not know their HIV status.
“We must train African spokespersons with African arguments to progress” Serge Douamong Yotta, Advocacy Director at Coalition PLUS
“Horizon 2030 will remain a beautiful dream if no diagnosis is made to identify pockets of resistance throughout the continent, and particularly in sub-Saharan and central Africa, analyzes Serge Douamong Yotta, director of advocacy at Coalition PLUS, an international federation of community NGOs. Many anti-LGBT movements have emerged, homophobia is unleashed: in Senegal, Burkina, Mali, Cameroon, South Africa. In Ghana, the law criminalizing homosexuality has been toughened. The UN strategy, which was based on tolerance, is outdated, because it is often perceived here as being imposed by the West. African countries will have to invest in the issue of sexual health and that of human rights for all. »
Discourses must therefore be developed on the continent itself so that appropriate solutions emerge. “Infected people must systematically be involved in the decision-making processes of the health programs that concern them, argues Serge Douamong Yotta. We must form African spokespersons with African arguments in order to progress. »
Peer educators, the keystone of the fight, must also be better trained and better paid, argue community associations. Meeting at the summit in Dakar, Senegal, in October 2021, they assessed the financial effort necessary for one third of the response budgets. Even if, recalls Pierre Mendiharat, “Without a vaccine, we will never beat HIV”. Since January, the Moderna laboratory has carried out three clinical trials of messenger RNA vaccines against HIV. A revolutionary biotechnology invented at the height of the Covid-19 crisis that sparked new hope of finally ending AIDS.
The key figures of AIDS in Africa
- Mortality Seven out of ten people who die of AIDS worldwide are African. Since the beginning of the pandemic, 36.6 million people have died from HIV. Since the peak in 2004, mortality has halved. In 2020, 680,000 people died of HIV-related causes worldwide, including about 500,000 in Africa.
- Hidden Scourge On the continent, a third of infected people do not know their HIV status.
- Cost The price of ARV treatment has dropped dramatically since its invention in 1996, dropping from over $10,000 per patient per year to $66.
- Treatment Of the 37.7 million people living with HIV, 27.5 million are on antiretroviral (ARV) treatment, an increase of 8.8% between 2019 and 2020, despite the Covid-19 crisis. Thanks to falling ARV costs, Africa is no longer an exception.
- Inequality Adolescent girls and young women in sub-Saharan Africa are twice as likely to contract HIV as men of the same age. Gender-based violence is the main cause of this over-contamination.
Summary of our dossier AIDS in Africa: the time of hope
This article is part of a dossier produced as part of a partnership with the Global Fund.