Flashes of light and black spots: A retinal detachment doesn’t cause any pain – that’s exactly what makes the visual impairment treacherous. It can be easily treated if the symptoms are recognized early. How does a retinal detachment become noticeable, what are its causes and how is the operation carried out?
- © Getty Images/Ivan Balvan
Quick overview: Frequently asked questions and answers
How can a retinal detachment occur? The most common causes of retinal detachment include tears or holes in the retina. Fluid can penetrate through this and cause the upper layer of the retina to separate from the lower one.
How bad is a retinal detachment? A retinal detachment is always a medical emergency and, in the worst case, can lead to blindness if no treatment is given. If you have any symptoms, you should visit an ophthalmologist immediately.
Can you cure a retinal detachment? The exact treatment depends on whether the eye disease is still in the early stages or has already advanced. If the retina has completely detached, the only solution is usually an operation with an inpatient stay.
Article content at a glance:
What is a retinal detachment?
A retinal detachment is a rare but serious eye disease. This results in a separation or lifting of the retina from the choroid. The technical term is Amotio retinae or Ablatio retinae.
The retina is located in the back of the eye and largely lines the inside of the eye. It is responsible for vision by processing light impulses and transmitting these signals to the vision center in the brain.
Important: A retinal detachment is always a medical emergency and can have serious consequences if left untreated. In the worst case scenario, there is a risk of loss of sight.
Different forms of retinal detachment
In general, the eye disease can have primary or secondary reasons. In secondary amotio, another disease is the cause.
Medical experts also differentiate between different types of retinal detachment. This includes:
Rhegmatogenous amotio: The most common form is caused by holes or tears in the retina.
Traactive Amotio: It arises from the pulling of connective tissue strands or scar strands.
Exudative amotio: The exudative form occurs when fluid from damaged vessels penetrates under the retina.
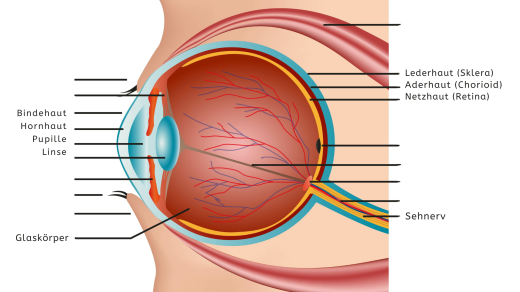
Structure of the eye: function of the retina
The eye is comparatively simple in structure: light falls through the pupil and casts an image of what is seen onto the back wall of the eye, somewhat like the inside of an old camera. Instead of the photographic film, the retina in the human eye absorbs the light.
However, this sensitive organ with millions of photoreceptors is not firmly attached to the rest of the eye, but rather adheres to its back wall with a kind of biological Velcro.
The vitreous body – the gel-like and transparent filling of the eye – ensures that the retina is always lightly pressed against this adhesive layer. In this way, the layer with the important photoreceptors is supplied with nutrients via the underlying layers of skin.
Retinal detachment: These symptoms are typical
The symptoms of a retinal detachment begin at the edge of the field of vision and expand from there. Signs that precede the actual separation often appear early on. If you notice the following warning signs, you should immediately consult an ophthalmologist or an eye clinic:
Flashes of light: The flashes of light appear when the eyes move and are caused by the stimulation of the sensory cells.
black spots: Those affected see numerous dark spots or dots (“soot rain” or “black swarm of mosquitoes”). They are the shadows of vitreous hemorrhages that occur when the retina tears.
bright flickering: It often only occurs on one side and is more pronounced in the dark than in the light.
If the retina is detached, further symptoms occur. This includes:
visual field loss: Those affected have the feeling as if a wall or a shadow were pushing in front of parts of their field of vision. Some report seeing a curtain or veil.
reduced vision: As long as only the periphery of the visual field is affected, vision is reduced. If the retinal detachment affects the center, visual acuity drops rapidly. Under certain circumstances, only light impressions can be perceived.
Retinal detachment can have various causes
Common causes of retinal detachment are degenerative changes in the peripheral retina and vitreous humor, which can lead to retinal tears.
A retinal tear occurs where the vitreous humor attaches to the peripheral retina. When the vitreous body becomes detached due to age changes, shortsightedness (myopia) (more than six diopters) or as a result of cataract surgery, a mechanical pull is created at the attachment points.
Gravity then pulls the age-related liquefied or restructured vitreous body downwards, which is why retinal tears occur much more frequently in the upper half of the retina than in the lower half.
In addition, vitreous fluid can penetrate into the area between the retina and the underlying pigment epithelium – these are the precursors to a retinal detachment. The detachment cuts off the supply to the photoreceptors and, in extreme cases, they die.
A special form of retinal detachment is the so-called giant ablatio, in which the tears extend over large areas of the retina.
Other possible causes of a retinal detachment
If the predisposition is hereditary, even a previously undamaged retina can tear. Retinal holes can also occur secondary to an eye injury during sports or bruises to the eye.
After the eye is bruised, for example as a result of an impact with a snow, squash or tennis ball, retinal necrosis occurs at the point of impact (parts of the retina degenerate and die), which can result in a retinal hole. Or, relatively soon after the accident, an acute detachment of the vitreous body with tearing of the retina occurs. However, it can take years until a retinal detachment occurs after a delayed tear.
Rather rare causes of retinal detachment are inflammation or tumors, such as choroidal melanoma. In addition, it can after
- unsuccessful retinal operations,
- shrinkage of the retina with secondary hole formation in diabetic retinopathy,
- after retinal vein occlusions and other forms of retinal ischemia as well
- as a late consequence of retinopathy of prematurity
retinal detachment occurs.
Diagnosis: How is a retinal detachment diagnosed?
If flashes of light suddenly appear, you should consult an ophthalmologist immediately – this is the only way to detect and treat an impending retinal detachment in a timely manner.
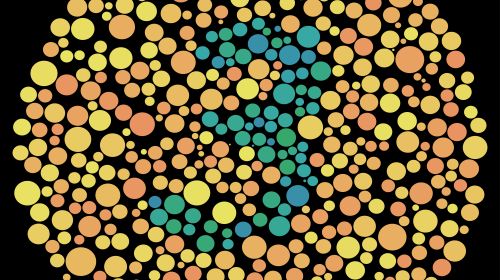
If a retinal detachment is suspected, both eyes are examined using an ophthalmoscope (indirect binocular ophthalmoscopy) and a contact lens. For this purpose, the pupils are dilated to the maximum using pupil-dilating agents. If the retina is severely detached, gray wrinkles or wavy displacement of the retinal vessels can be seen.
The cracks are usually in the shape of a horseshoe or a shark’s mouth. Sometimes peripherally located round holes can also be seen.
A so-called flat or circumscribed retinal detachment is more difficult to detect. The retina is usually still transparent, which is why you have to look carefully for a retinal tear. Careful documentation is important and serves subsequent therapy.
Furthermore, a distinction must be made between diseases such as:
- uveal melanoma,
- of vascular tumors of the retina,
- a peripheral retinal split or
- necessary for Harada’s disease,
as these can be very similar to the clinical picture of a retinal detachment.
Treatment of retinal detachment: surgery or laser
There are several ways to treat a retinal detachment. The type of therapy depends on the extent to which the retina has been damaged and what triggers are present. If underlying diseases are the cause, they must be treated.
In the early stages, i.e. when the retina has not yet completely detached, treatment can usually be carried out on an outpatient basis.
Only when the retina has detached will an operation and hospitalization be necessary. The doctor puts the retina back in the right place. As a result, the supply to the receptors is restored, which means vision returns.
The following treatment procedures are possible, among others:
Laser treatment: Smaller tears or holes can be treated with a laser. The retina is connected to the choroid and thus prevents detachment.
Surgery with cold probe: The so-called cryopexy is used when laser therapy is not possible. The goal of this retinal surgery is to freeze tears.
Denting surgery: The eyeball is dented slightly using a seal or cerclage made of silicone. A cerclage is more like a loop, a seal is more flat. They are attached to the sclera (outermost layer of the eyeball). The external pressure pushes the retinal layer back into its original position.
Removal of the vitreous body (vitrectomy): A common surgical method is removal of the vitreous body. It is replaced with a saline solution, gas, air or silicone oil. In this way, the retina returns to its original position.
A combination of vitreous removal (vitrectomy), denting surgery and internal tamponade is necessary if complicated retinal detachments or a giant tear ablation are present.
Prognosis: Can a retinal detachment be cured?
The smaller the retinal detachment and the sooner the retina is reattached, the better the treatment and therefore the prognosis. Serious consequences such as blindness can then be prevented in many cases.
In the case of uncomplicated retinal detachment, in 85 to 95 percent of cases it is possible to reattach the retina through denting surgery.
How much visual acuity is still possible depends on how long the macula (area of sharpest vision) was lifted, as the sensory cells located in the macula were not nourished during this time and were therefore damaged.
After a retinal detachment with prolonged macular detachment, it can take a year until the maximum achievable (final) visual acuity is achieved.
Prevent retinal detachment with regular check-ups
If the first eye becomes ill, the second, healthy eye should be examined to avoid further retinal detachment.
Adults should have regular checkups. Experts recommend a check-up at an ophthalmologist’s office every two years for those age 40 and over. Children and adolescents are less at risk because their vitreous body still has a firmer consistency.
Nearsighted people should get preventive care earlier and more often because they have a higher risk of retinal damage. Another risk factor is diabetes mellitus. Diabetes changes the composition of the vitreous body.
Anyone who is unsure whether they are suffering from a retinal detachment should always seek professional advice: abnormalities can often be identified and treated at an early stage.