Hemorrhoids seal the anus from the outside. If they are enlarged, they cause unpleasant symptoms such as itching, burning or stool soiling. Various treatments, from home remedies to ointments to surgery, can help.
- © iStock.com/fizkes
Quick Overview: Hemorrhoids
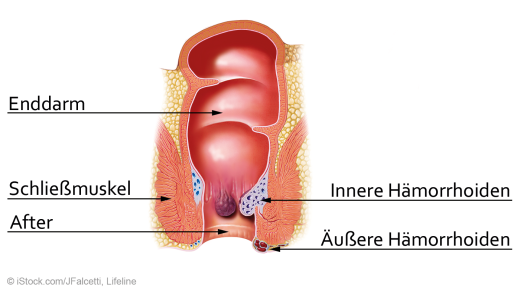
Definition: Hemorrhoids are vascular cushions in the area of the rectum at the transition to the rectum. When they are enlarged, they become noticeable as nodular bulges of certain blood vessels.
Symptoms: Itching, burning and weeping in the anal area and bright red blood on the toilet paper are typical.
Treatment: Depending on the degree, ointments and suppositories with lidocaine or cortisone, sclerotherapy or rubber band ligation can be used. In severe cases, the enlarged hemorrhoids may need to be surgically removed.
Causes: They are often triggered by straining when having a bowel movement, persistent constipation or excessive use of laxatives.
Diagnosis: The first point of contact is a proctological practice, where a physical examination and mirroring of the anal canal takes place.
Article content at a glance:
What are hemorrhoids?
Hemorrhoids are a normal and important part of the body. The vascular cushions are ring-shaped cavernous bodies in the anal area, which are located at the transition from the rectum to the rectum. Together with the sphincter, they serve to seal the anus and thus prevent fecal incontinence.
Hemorrhoidal cushions are erectile tissue that fills with blood to seal the anus. They are pushed aside during defecation. In the case of enlarged hemorrhoids, the blood accumulates and the venous drainage is impeded.
Different stages
Depending on their severity, enlarged hemorrhoids are divided into four grades or stages:
Stage I: In the first stage, the hemorrhoids appear internally and are therefore only visible through an examination of the rectum (proctoscopy).
Stage II: The hemorrhoids protrude from the anus during bowel movements and are then visible. Afterwards they withdraw again.
Stage III: The hemorrhoids pop out when you strain, but they don’t go away on their own. However, they can be pushed back into the anus with a finger.
Stage IV: If the hemorrhoids are permanently fixed outside the anus, the fourth stage has been reached. They can no longer be pushed back either.
What are signs of hemorrhoids?
If the vascular cushions cause problems, this is referred to as haemorrhoidal disease. This is widespread: it is estimated that around 80 percent of adults in Germany suffer from enlarged hemorrhoids at least once in their lives. Then the knots often prevent a complete sealing of the sphincter to the outside. Traces of faeces (stool smearing) and mucous secretions from the intestine irritate the sensitive anal skin.
Typical symptoms:
- itching
- Burn
- oozing
- Feeling of incomplete evacuation of stool
- anal eczema
- bright red blood on the toilet paper
Pains
Ointment, suppositories, sclerotherapy: what helps with hemorrhoids?
The treatment of enlarged hemorrhoids depends on their severity. Whether hemorrhoids are also treated at an early stage depends on the individual suffering. On the other hand, if left untreated, severely enlarged hemorrhoids can lead to anal thrombosis or anal fissures over the long term. Both diseases are rather harmless, but painful. Heavy, continuous bleeding from hemorrhoids can also cause anemia.
Ointment and suppositories: Anti-inflammatory and pain-relieving ointments or suppositories, for example with the low-dose active ingredients cortisone or lidocaine, are usually sufficient in the first stage. However, they can at most alleviate symptoms such as itching in the anal area; they have no influence on the size of the hemorrhoids. In the case of pronounced anal eczema, which often occurs in connection with hemorrhoids, prescription cortisone ointments are usually used. In order to work optimally, suppositories are placed about two centimeters behind the anus.
Sclerotherapy (sclerotherapy): It involves injecting a vaso-sclerosing solution, usually alcohol, into the tissue around the enlarged hemorrhoid. It causes a local inflammation, as a result of which the blood flow to the affected area in the anal area decreases. The minimally invasive treatment can be carried out on an outpatient basis. Three surgeries spaced four to six weeks apart are common. However, the procedure is unsuitable for inflammation or pregnancy.
rubber band ligation: The hemorrhoids are tied off with a rubber band. Due to the lack of blood supply, the tied tissue knot dies after three to ten days and is excreted. This creates a wound that takes three to four weeks to heal. Only then should another ligature be made. The procedure is considered to be low-risk. Temporary pain may occur, and bleeding is rare. The ligature has a higher chance of success than sclerotherapy: 70 percent of the patients are free of symptoms even after five years.
Hemorrhoidectomy: Surgical removal is advisable from the third stage. The most common methods are the Milligan-Morgan and Parks methods, each named after their inventors. In both cases, the three largest knots are cut out. With the Parks operation, however, the wound is almost completely closed, while with the Milligan-Morgan method it remains open and can sometimes cause great pain, especially during defecation. Another procedure, Ferguson’s surgery, aims to completely close the wound but increases the risk of bruising under the skin.
Home remedies and tips for hemorrhoids
Some home remedies alleviate typical symptoms such as anal eczema, itching and burning in the anal area or even make hemorrhoids disappear completely:
Ensure soft stools, tips for a healthy daily diet, drink enough (at least 1.5 liters per day) and move a lot.
Sitz baths, for example with oak bark, witch hazel, yarrow, horse chestnut or chamomile: This is how the medicinal plant works on the skin and stomach, alleviating itching and inflammation. A sitz bath should be at body temperature and last about three to five minutes. If there are signs of an allergic reaction, which occur occasionally, you should stop using the active substance in question.
Clean the anus gently with lukewarm water, for example using a cotton pad. Then gently pat dry.
It is best to use soft, unscented toilet paper.
If you have problems with stool smearing (some feces come out of the anus after a bowel movement), place a cotton pad between your buttocks after going to the toilet. This prevents irritation of the sensitive anal skin, one of the main causes of anal eczema in hemorrhoids.
In phytotherapy, teas are also used to treat hemorrhoids. Suitable active ingredients are celandine, rhubarb and horsetail.
An anal dilator can be used to prevent mild hemorrhoids. The cone-shaped instrument is carefully inserted repeatedly into the anal canal with a little lubricant. This stretches the anal sphincter muscles. In addition, the sphincter muscle can be contracted against the resistance of the anal dilator when it is fully inserted. To prevent injury, medical advice should be sought before use.
What causes hemorrhoids?
It is estimated that half of all people over the age of 30 are affected by enlarged hemorrhoids. And they are also increasing among younger people. In most cases, several risk factors such as malnutrition, obesity and lack of exercise come together. However, the trigger for the enlarged vascular cushion is usually strong straining during a bowel movement, caused by constipation and constipation.
Risk factors at a glance:
frequent constipation (hard stools)
mostly sedentary work
low-fiber diet
frequent suppression of the urge to defecate (holding in the stool)
overweight
pregnancy and childbirth
congenital weakness of the connective tissue
long-term very soft stool
Diagnosis of suspected enlarged hemorrhoids
In order to determine the stage of the hemorrhoids, the proctological doctor will first discuss the medical history and symptoms as part of the anamnesis. This is followed by a physical examination and a finger palpation of the rectal area. In men, the prostate is also scanned. The functionality of the sphincter can be checked by pressing at the same time.
In addition, a proctoscopy (anal canal reflection) is required. An eight to 15 centimeter short, tube-like tube is inserted into the rectum. The proctoscope is equipped with a light source and allows a precise examination of the rectum. The procedure itself is painless and only takes a few minutes. As a result, no sedatives or short anesthesia are usually necessary. The proctoscopy is performed in the knee-elbow position (on all fours), on a gynecological examination chair (lithotomy position) or on an examination table.
In addition to the anal canal endoscopy, a colonoscopy or rectoscopy can also be performed. These diagnostic procedures are mainly used to rule out colon cancer and a higher source of bleeding.
These measures prevent hemorrhoids
One of the main causes of haemorrhoids is hard stool and the associated straining, which causes the vascular cushions to swell. Regulated digestion is important to prevent symptoms.
Diet has a decisive influence here: A balanced, mixed diet rich in fibre, as well as drinking a sufficient quantity of at least 1.5 liters of water or unsweetened tea daily ensure soft and regular bowel movements.
Foods that have a positive effect on digestion in hemorrhoids:
- whole grain products
- fruit, vegetables, salad
- legumes
- Berry
- nuts
- Dairy products such as buttermilk, kefir or yogurt
- Muesli, oatmeal (preferably natural)
- Linseed, psyllium husk
- plum juice, sauerkraut juice
- Apple Cider Vinegar
Physical activity also stimulates intestinal activity. However, when exercising, people with enlarged hemorrhoids should make sure that they choose sports that do not strain the pelvic floor. Because this puts additional pressure on the vessels in the anal area, so that hemorrhoids can be aggravated. Unfavorable sports units include strength training, jumping rope, tennis, squash or football.
Gentle movement sequences are more suitable for hemorrhoids:
Sometimes constant stress or certain medications are to blame if the intestines become sluggish.